Filler-related blindness is a very rare but serious complication that both the injector and patient should know about before any filler is injected into the face.
Although there are less than 100 cases reported in the literature, according to the most recent global review, the actual number is probably closer to 300-400 cases globally, with the first known filler blindness case in NZ last year, and in Australia this year.
When you consider that there are hundreds of millions of filler treatments performed globally each year, filler blindness is a very rare side effect – but a very serious one.
It’s believed that the reported rate has risen due to the increasing popularity of facial fillers, increased awareness and hence reporting, and also as a result of the areas of the face that are now injected with fillers.
Dermal filler blindness FAQs
1) Of the reported cases, which area is the highest risk?
Of the 98 cases reported by Belezeney in 2015, the nose and frown region made up 63.5% of the cases, and the nasolabial fold was the next highest at 13.3%, but filler blindness has resulted from filler treatments in almost every area of the face.
2. How can you prevent filler-related blindness?
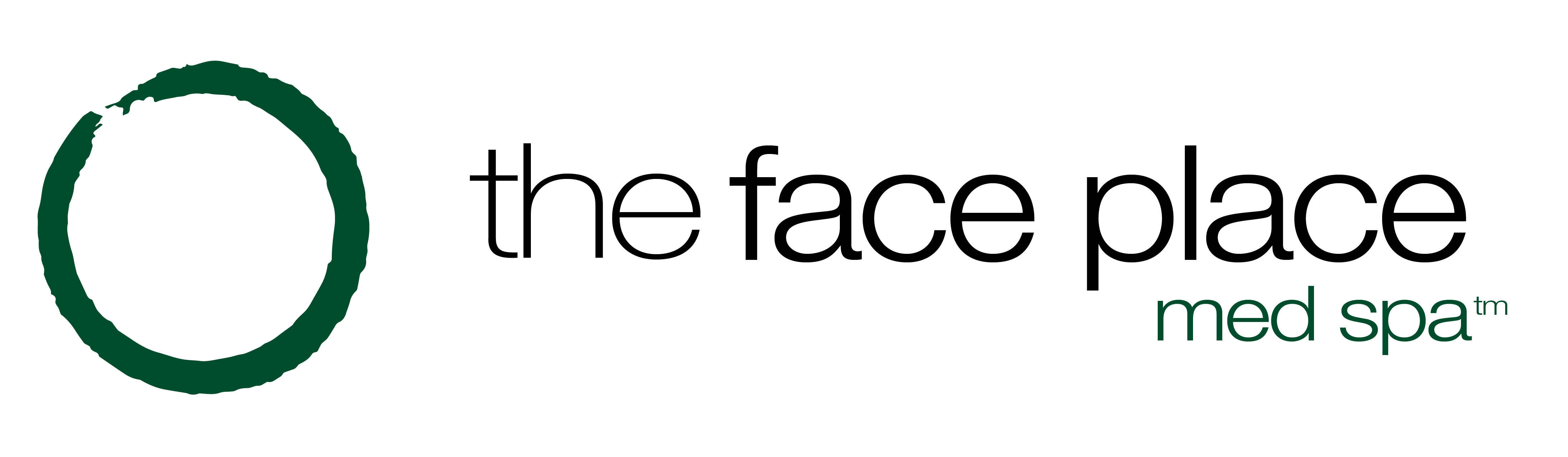
At The Face Place, the risk of blindness and how we manage it is discussed with every client before we proceed with dermal filler treatment. Having an extensive awareness of facial arteries and human anatomy is vital to reduce the risk of blindness. Prevention is always the best treatment!
3) How can we treat dermal filler-related blindness?
We have a full written protocol which is practiced at least every 6 months. If we are unlucky enough to have a case despite all the preventive measures we use, the first thing we would do is call our dedicated emergency eye specialist to let them know we will be with them within 30 minutes and to be ready for us. The injector would notify reception, and our reception team have a prepared script so that no important information is missed.
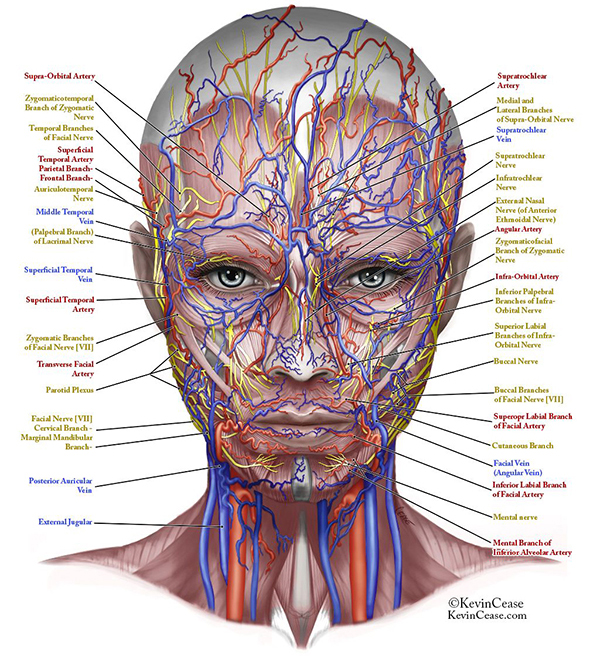
We would then assess the person’s vision, and inject Hyalase into an easily accessible blood vessel above the eye, which connects with the internal carotid system – as well as any areas of blanching – while the taxi or Uber is being called. If there is time, photos are taken.
It is thought that breathing into a paper bag can increase the CO2 in the blood and cause the blood vessels to dilate (open wider), so we would start this as quickly as possible, along with a special type of pressing massage to the eye to attempt to dislodge the clot and/or move the Hyalase into the blockage.
We send the clinician with the patient along with their notes and 2-4 extra vials of hyalase, so that the eye specialist can perform retrobulbar (behind the eye) injections of the hyalase immediately when we get there.
There are some clinicians who might attempt this injection themselves in the clinic, but this is not an injection we are trained in or do regularly, and there is a chance of perforating the eyeball if not done correctly, which is why we get an eye specialist to perform the procedure. The eye specialist can then also perform any additional tests or treatments that might be required.
4) How can dermal filler cause blindness?
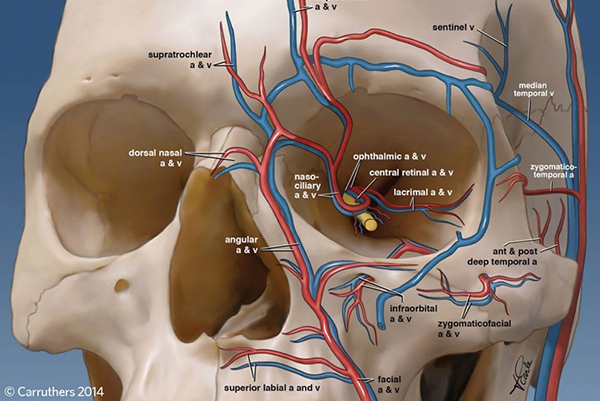
To cause filler blindness, you need to penetrate an artery (which is usually pretty hard to do), and then inject enough product, with enough force, that it blocks the artery against the flow of blood, and extends back up to block the artery that supplies the eye – the retinal artery – which is part of the internal carotid artery system.
There are key arteries in the face that anastomose (join up) with the internal carotid system, and while there are key risk areas, everyone’s anatomy is different. An experienced and educated injector will be aware of the high risk areas, how to recognise the onset of blindness, and how to manage it. Even though this is very rare, we recommend that every clinic has a written protocol to manage the complication, and role play the management regularly with their whole team.
In the 2015 review, the most severe cases were from fat injections and other non-reversible fillers. Complete blindness occurred in 47 cases, and there has also been a case reported where, sadly, both eyes were affected.
Fortunately, if reversible HA (Hyaluronic Acid) fillers are used, there is a higher likelihood of being able to reverse filler blindness if hyalase – the enzyme that dissolves HA filler – can be injected into and around the internal carotid artery system within 30 minutes.
5) Has filler-related blindness been reversed?
There are now at least 2 cases where reversal of filler blindness has been reported in the literature – one by a friend of mine in Australia, who injected hyalase into one of the blood vessels that connects with the internal carotid artery system, and one with retrobulbar (behind the eye) hyalase. Both had treatment within 30 minutes of developing symptoms.
6) How do I know whether the dermal filler has blocked an artery?
Signs of filler blindness usually include a searing, ripping pain (but not always), and blanching (whiteness) of the skin in the area supplied by the artery. Loss of vision usually occurs within minutes and may be accompanied by the eye getting ‘stuck’ in position.
To reduce the chance of causing this serious side effect, we use small amounts of filler injected very slowly, and we aspirate (pull back the plunger to create a vacuum which will pull blood into the syringe if we are in a blood vessel) before injecting in some of the high risk areas.
Some clinicians believe in aspiration, and others do not – it is an ongoing debate at every major conference – I figure that we should do everything in our power to prevent this devastating side effect from occurring. Many clinicians also do not aspirate properly – the plunger must be pulled back at least 10% of the syringe volume (ideally 20%) and held for at least 6-10 seconds depending on the type of filler and type of needle being used.
7) What should I consider before having a dermal filler treatment?
If you are considering a facial filler treatment, please make sure that your clinic:
– discusses the risk with you, along with how they avoid it and what they would do if it occurred
– has hyalase in the room while injecting, and it is within the expiry date
– has a written protocol on how to manage the complication should it occur
– has a relationship with an eye specialist experienced in this particular issue that they can get you to within 30 minutes if required
We sincerely hope that we never have to deal with a case of filler-related blindness, which is why we do everything in our power to avoid it. Although it is very rare, it’s a serious and important concern to know about, and consider before any filler treatment.
This is a scary complication for everyone, including the injector, so we hope that sharing our protocol (taken from the latest best practice recommendations) helps to provide education to both patients and the industry so we 1) reduce the chance of it occurring, or 2) increase the chance of regaining eyesight if it does occur and is managed appropriately.
If you are a clinician (doctor or nurse) looking to invest in your patients’ safety, check out our Hyalase Workshop where we hold an intimate, practical workshop on Hyalase and dermal filler safety. From safety training to advanced injecting, we cover all the difficult areas to treat and how to act should something go unfavorably.
Warmest regards,
Dr Cat